Addressing the Most Critical Factors Toward Eliminating Diseases of Poverty
 Professor Bentwich, a physician, and world-renowned clinical immunologist and AIDS researcher. Since its onset, he became involved in AIDS and AIDS research and led the first AIDS center in Israel. Currently, he is Professor of Microbiology and Immunology at the Ben Gurion University in Beer Sheba, where he is also head of the Center for Tropical Diseases and AIDS (CEMTA) and its implementing arm in Africa –NALA Foundation, that is heavily involved in eradicating Neglected Tropical Diseases from Ethiopia and Africa. In the course of the last five years this activity has covered a population of over five million people and is about to expand and reach several millions by the end of 2021. Prof. Bentwich is author of 280 scientific publications in peer reviewed journals and is a member of several editorial boards of leading journals, as well as being member of several medical scientific societies.
Professor Bentwich, a physician, and world-renowned clinical immunologist and AIDS researcher. Since its onset, he became involved in AIDS and AIDS research and led the first AIDS center in Israel. Currently, he is Professor of Microbiology and Immunology at the Ben Gurion University in Beer Sheba, where he is also head of the Center for Tropical Diseases and AIDS (CEMTA) and its implementing arm in Africa –NALA Foundation, that is heavily involved in eradicating Neglected Tropical Diseases from Ethiopia and Africa. In the course of the last five years this activity has covered a population of over five million people and is about to expand and reach several millions by the end of 2021. Prof. Bentwich is author of 280 scientific publications in peer reviewed journals and is a member of several editorial boards of leading journals, as well as being member of several medical scientific societies.
The genesis of how NALA came to exist is quite unique. Your medical practice was originally focused on HIV. How did you become focused on solving the Neglected Tropical Diseases (NTD) problem? What is the relationship between HIV and NTDs?
The short answer is relatively simple, because of the wave of immigration of Ethiopian Jews from Ethiopia to Israel in 1991. At that time, something like two percent of the immigrants had HIV, and this did not prevent their coming to Israel. However, once they came into Israel, several hundreds of them were sent over to my AIDS center for treatment and care. Early on, I became aware that in addition to HIV, most of them were also infected with intestinal worms. Actually, several kinds of worm including schistosomiasis (schisto), or bilharzia, as well.
Being an immunologist, this observation led me to ask the question of whether these co-infections, which obviously were very widespread in Ethiopia, could influence the immune system — thereby influencing the susceptibility to get infected with HIV, and also weakening the ability to cope with the infection. As a result, I carried out a number of studies on other Ethiopian immigrants that did not have HIV — but did have intestinal worms.
To make a long story short, our studies did show that intestinal worms have a very significant impact on the immune system. That led us to suggest that they play a very important role in HIV/AIDS in Africa, and other developing countries. The implication of this finding was that you have to get rid of these infections if you want to fight or diminish the spread of HIV.
Remember, we are talking about the ’90s, and the issue of why HIV/AIDS was behaving differently in Africa than in Europe or the USA was a major and very intriguing question. What we uncovered drew a lot of attention. However, the publication of these findings came at the same time that the antiretroviral cocktail became known, and was also proven to be very effective in the treatment of HIV. This pushed aside our findings and certainly diminished the interest in controlling intestinal worms, let alone the fact that Africa was not the center of interest for HIV/AIDS care.
When I went to Ethiopia to start eradicating intestinal worms, something like 14 years ago (2006 or 2007), nobody was really interested. Not only were they not interested, but they thought it was unrealistic to try and control these diseases because they were facing AIDS and malaria, and these were much higher on their agenda than dealing with NTDs. It was only in 2013 that these diseases were starting to be discussed and made any kind of priority by the Ministry of Health or other health organizations.
There is certainly a traditional idea of viewing NTDs as relatively minor, regional problems. They are highly treatable, and labeled ‘neglected’ tropical diseases for a reason — because they are virtually unknown in more affluent nations. What is the problem with looking at diseases and epidemiology in this way?
In America, if you talk about parasites or intestinal worms, people get so disturbed, they cannot digest that term. That gave rise to the term neglected tropical disease. It also gave us sort of a common denominator, or common name, across various widespread issues. It covers several diseases, more than just intestinal worms. The advantage of calling them all neglected tropical diseases lies in what is common to all these diseases — these are all diseases of poverty.
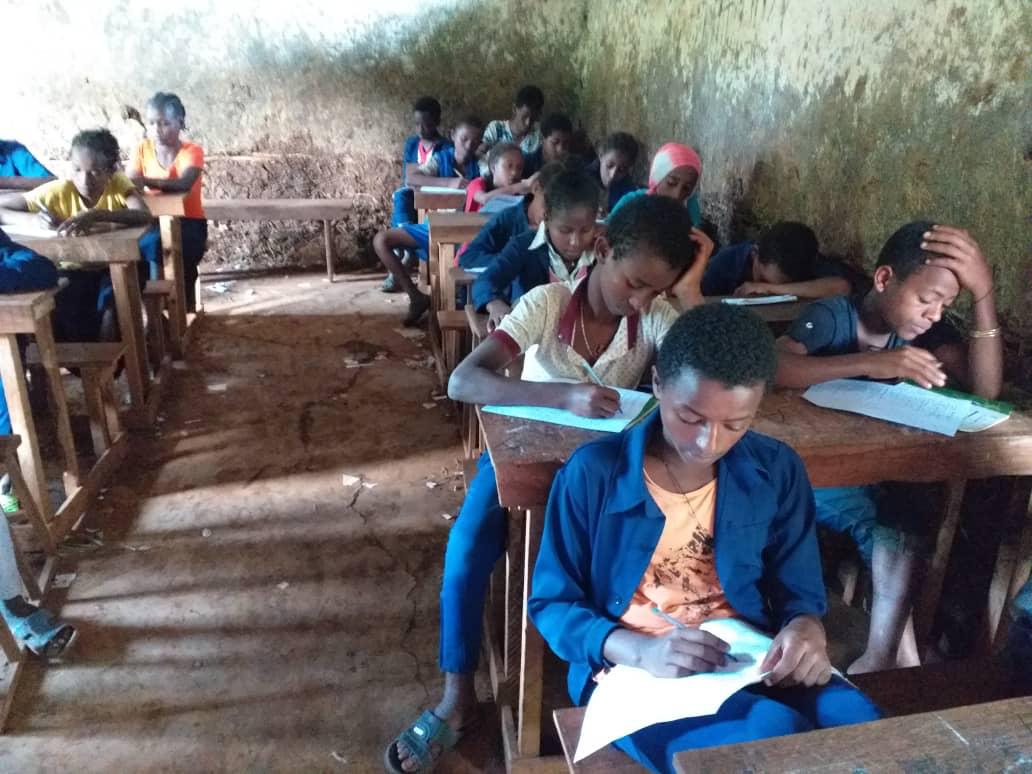
All of them result from poverty, and low socio-economic situations. They also aggravate poverty. When people have these diseases, they are less able to work, less able to function, and less able to study — and that obviously aggravates their situation. Poverty is therefore the common denominator of these diseases. It is also worthwhile using the term NTD for motivating the changing and improving the situation, which is key for the further development of these populations. You can generalize and say that applies to all developing countries, and is a universal issue.
NTD, Advocacy, Learning, Action (NALA) successfully eliminated schistosomiasis from schools in Mekelle, Ethiopia in six years. What have you learned about how to effectively achieve resilience and eradicate these diseases? How can this be replicated in other places? Why are traditional remedies, such as massive drug administration, not sustainable long-term solutions?
 We now have a follow up at ten years after our first intervention that will be published soon. We went back to Mekelle and looked at the same ten schools that we worked with ten years ago. It is, of course, a limited sample, but it’s definitely representative. Out of these ten schools, in seven — that’s 70 percent — schisto infection rates remained very low, below 2%, compared to the mean of 60% before the intervention! This demonstrates very clearly the success of our intervention and how well this achievement has been sustained and maintained. However, in three out of the 10 schools, there was a recurrence of the infection and this raises the obvious question of why these three schools were not as successful as the others.
We now have a follow up at ten years after our first intervention that will be published soon. We went back to Mekelle and looked at the same ten schools that we worked with ten years ago. It is, of course, a limited sample, but it’s definitely representative. Out of these ten schools, in seven — that’s 70 percent — schisto infection rates remained very low, below 2%, compared to the mean of 60% before the intervention! This demonstrates very clearly the success of our intervention and how well this achievement has been sustained and maintained. However, in three out of the 10 schools, there was a recurrence of the infection and this raises the obvious question of why these three schools were not as successful as the others.
Other organizations and NGOs had been trying to eradicate or treat intestinal worms and schisto at the same time as we did in Ethiopia. At that time, one thing struck me clearly about their approach — they were using only mass drug administration for that purpose. They were using drugs that were effective against the worms, and were doing so once or maybe twice a year. But they were not changing the poor infrastructure, and not addressing the behavior of the population. In other words, infected people would get the medication, it would cure their infection for a period of a few weeks or maybe months, but then they would get infected again. If you are not changing the behavior of the people; what do you expect? If they don’t change their behavior, they will get exposed again and will get reinfected.
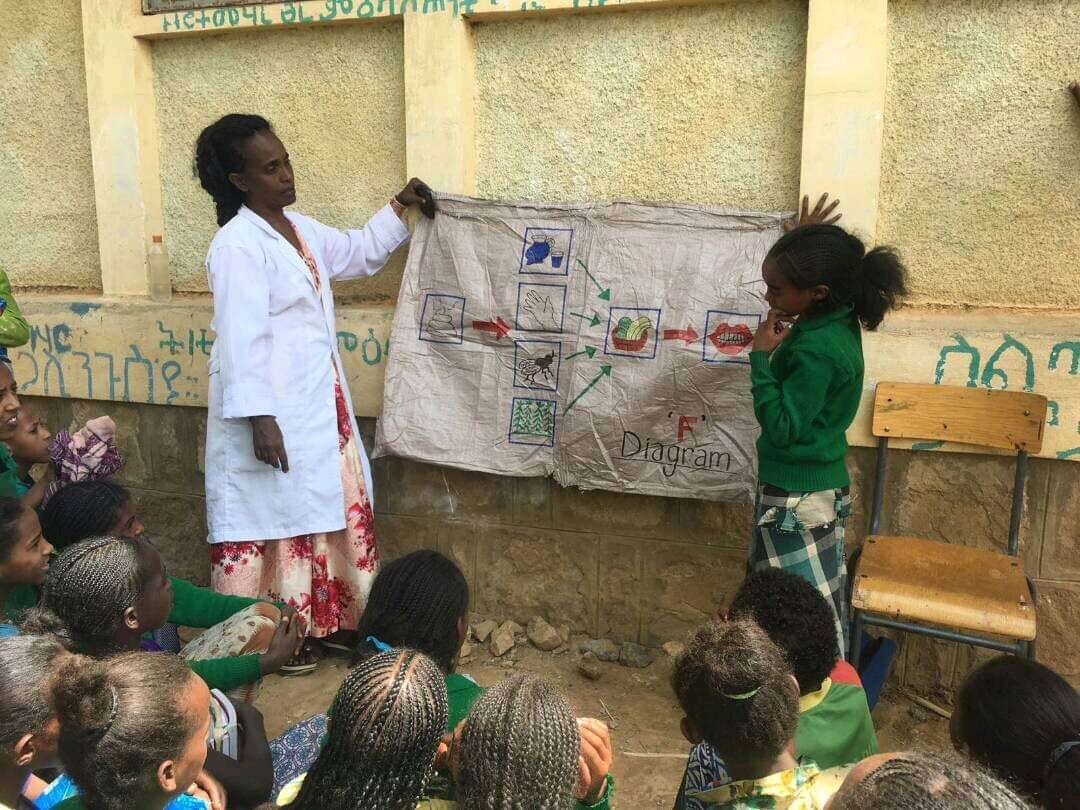
This led me to understand that the rationale and objective of our intervention, and also the possible advantage of our organization would be changing behavior, not just administering medication. Everything can be achieved if you change behavior. The best way to express this success and ideology is ‘comprehensive community-focused work.’ In other words, you approach the whole community. You need to have the teachers, the parents, supporting community organizations, all committed to that objective. For instance, if you have latrines and they are not well-kept; they get blocked or clogged so they cannot be used — then you very much need that community to feel a sense of commitment, and obligation, and responsibility. Believe it or not, even the poorest people were happy to give small sums of money for a janitor and to keep the water running. It is a process, not just one element that made it work.
I want to re-emphasize, or reinforce, the need to get motivation. You cannot get this unless people are convinced or committed that this is worthwhile. You need messengers. The best messengers are from within the community and leadership. It cuts more than one way. You have to find the right messenger; children are very good messengers. One more example, in Ethiopia there is the Women’s Volunteer Army. It was established to get women committed to help in achieving goals that are important for the state’s higher levels. There is a whole hierarchy throughout Ethiopia of women’s groups that are committed to doing things for the community. They became a very important force because women are in charge of the household, so they carry a lot of influence and impact.
The global COVID-19 pandemic has exacerbated multiple existing problems in Ethiopia. Specifically, there is a dire impact on education — which is a central force in changing behavior. Schools across Ethiopia have been shut down due to a lack of adequate capacity for necessary hygiene measures. (If children are not in school getting educated, it can set the country back even further for many decades. This is arguably the most critical secondary impact of the pandemic.) Can you describe the compounding effect of now having to confront COVID in addition to NTDs?

Where we can really claim originality and achievement, is primarily in behavior change. We have also developed tools to improve the coordination between various authorities — such as those that deal with WASH, that is primarily water and sanitation, and the authorities that deal with the diseases themselves. It is easy to imagine how coordination is a major obstacle. You have to develop tools for how you can achieve optimal coordination between all of the different authorities that are trying to address these problems. That applies also to COVID, obviously. In Ethiopia, for the next five years, we are looking to address these issues nationally, not only regionally.
NALA is currently scaling operations and working with the Bill and Melinda Gates Foundation on an initiative that will provide a multi-pronged solution to take on NTDs, COVID-19, and their related WASH issues all at once. Innovation is rapidly becoming a critical factor in solving these expanding issues that are rooted in poverty. Where/how do you see NALA innovating and meeting the growing challenges during the next five years?
The Gates Foundation put out a call for applications that would show innovation in the struggle against COVID, related to the outcome of the work with NTDs. Our experience with NTDs was therefore very relevant to COVID and something that can be easily applied to COVID. Based on our experience in the schools, we found that the availability of water was not simply based on the water supply. You might have 100 schools without running water, with no water flowing from the taps — though there was no shortage of water in the area.
The obstacle was mostly the maintenance of the water supply system. It would be the pump that doesn’t work, or the pipes that are clogged; all of which can be easily fixed with a technical team. What you need is a technical team that can usually solve the problem in a very short while. We came up with a novel suggestion for mobile maintenance teams that would spend a day in each school looking into the maintenance problems. They would solve the problem, and water will be flowing through the taps. You don’t need a million dollars — you need just a few thousand dollars to make this work. And indeed, we won that award, which will support one such mobile unit on wheels for a year. When we show the effectiveness of this approach, we hope it will be extended and expanded into other areas in Ethiopia, and maybe elsewhere.
As we look to the future, there are major elements that we are trying to develop. One is to start applying our experience and contributions to other countries. Another is for us to establish a Training and Innovation Center of Excellence for instruction and the dissemination of lessons that we have learned, and for training other teams in Ethiopia and Africa. It would hopefully be a collaboration with the Yale School of Public Health, which would bring the academic support of an American established institution. I think one of the weak elements in NALA has been the paucity of publications that demonstrate our achievements, and help in disseminating this information beyond Ethiopia. We certainly need to expand on that. We need to disseminate information in a much more significant way. That is a very important objective.
What concerns you most about the world today, and what brings you hope?
The phenomenon of leadership that threatens our democracy, to our basic values, is a serious one. It is a leadership and human rights crisis. For many years, I’ve been the chairman of the Physicians for Human Rights in Israel. Human rights concern me a lot. I grew up on the idea of Tikkun Olam. It’s one of the things we should do throughout our lives, and I am very happy that I am doing my best on that account.
My HIV/AIDS experience has been very revealing and rewarding, and extremely pleasing in the sense that I was there from the beginning. We never expected to see such an epidemic. It was a very threatening and extremely difficult situation. The achievement in the fight against AIDS has been extremely successful; from a disease that almost everybody died from, people don’t have to die from AIDS anymore!
Taking that experience and applying it to the NTDs — If you were to ask me 10 years ago, maybe even seven years ago, about the prospects for these diseases, I would have been much more pessimistic than I am today. It is not an unrealistic dream or hope that within between 10 and 20 years, these problems will be significantly diminished. This is very encouraging. If I look ahead, yes, it is achievable. Will it be solved in 10 years? Probably not. Maybe not even in 20 years, but in 30? Yes, certainly for schisto and Trachoma. That is a very optimistic and hopeful vision.
To learn more about the NALA Foundation, visit their website at https://www.nalafoundation.org/









Got something to say?